September 7, 2024
Urinary System Incontinence In Women
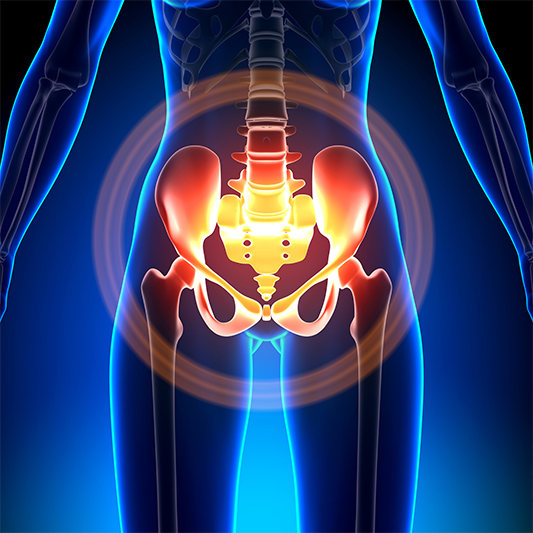
5 Factors For Urinary System Incontinence In Women: Florida Lady Treatment Of Jacksonville: Obgyns Regardless of the kind or intensity of the disease, it is suggested that patients have behavior modification, which involves a adjustment in way of living. Overweight persons' treatment of UI need to start with weight decrease of a minimum of 5%. Recent scientific records indicate that weight reduction of 5% causes a reduction of objective signs of SUI. Not without significance is to control the time and quantity of Click for info liquid consumption. It is additionally advised that clients with incontinence discontinue exercising sporting activities that negatively influence the pelvic flooring muscles such as exercises on trampolines.Medical Professionals
The decrease in women hormones may present you with various possible problems and negative effects, including female urinary incontinence (UI). It is estimated that in between 3 and 6 million individuals in the UK suffer from urinary incontinence. With majority of postmenopausal women suffering from some degree of UI. Adding in anticholinergic drugs can assist along with bladder training and weight loss. These medications intend to lower the contractions of the detrusor (bladder wall muscle mass). Some of these medications can be quite costly as not every one of them are readily available on the Drug Perks System (PBS).Selecting The Appropriate Female External Urinary System Catheter For Home
What foods cure urinary incontinence?
Bananas, apples, grapes, coconut, and watermelon are excellent choices for those with overactive bladder. Vegetables & #x 2013; Leafy environment-friendlies, like kale, lettuce, cucumber, squash, potatoes, broccoli, carrots, celery and bell peppers. Whole grains, like oats, barley, farro, and quinoa (additionally a fantastic healthy protein).
- Urinary system urinary incontinence (UI) is an essential social problem that impacts greater than 50% of postmenopausal females [4]
- These adjustment can make it testing to invalidate your bladder and quit urine from dripping out.
- Your bladder resembles a tank-- when the bladder is complete, the mind sends out a signal that it's time to pee.
- Treatment alternatives for menopause incontinence consist of Way of life and Behavioural Modifications, Bladder Training, and Pelvic Floor Muscle Mass Therapy, among others.
Social Links