September 11, 2024
Did You Understand Hormonal Inequality Can Affect Bladder Health?
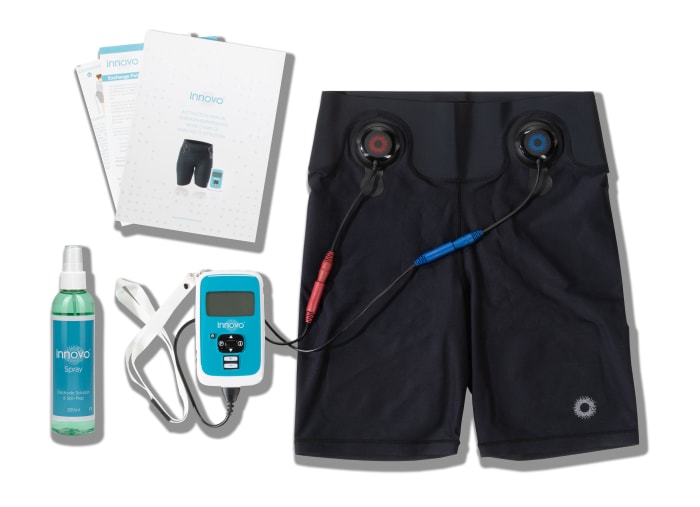
The Duty Of Hormones In Female Urinary Wellness Although its usage in the therapy of vaginal degeneration is well established, the impact of HRT on urinary system continence is debatable. In this paper, we will review these recent researches and take a look at the evidence for the effects of estrogen on the postmenopausal urogenital tract. This sort of incontinence typically arises from compromised or harmed pelvic floor muscles, which are unable to sustain the bladder and urethra sufficiently. As the womb enlarges to suit the expanding fetus, it exerts increasing stress on the bladder and pelvic floor.- One of the most effective means to stay on top of urinary system incontinence is with the use of grown-up diapers for women.
- Some common negative effects of mirabegron include nausea, looseness of the bowels, constipation, lightheadedness and headache.
- Furthermore, prolapse of the former vaginal wall surface can affect bladder draining.
- Private incontinence conditions, treatment and healing times may differ.
- As you age, your estrogen degrees decrease significantly-- specifically during menopause.
Just How Is Urinary Incontinence Diagnosed?
Paraplegia or quadriplegia can establish within hours or days after the first neurologic shortage shows up. Laxity of the pubourethral ligaments (ie, anterior zone of damage), mid vaginal area (ie, center zone), and uterosacral ligaments (ie, posterior area) make the normal tridirectional assistance of the vagina ineffective. Hemorrhage, infarction, or vascular concession to certain areas of the mind can cause reduced urinary system system dysfunction. The frontal lobe, internal capsule, brainstem, and cerebellum commonly are included sites. At first, urinary system retention as a result of detrusor areflexia is observed. In combined incontinence, the bladder outlet is weak and the detrusor is overactive. When this occurs, you might really feel the demand to void more often, which is the primary signs and symptom of OAB. In this short article, we will explore reduced estrogen bladder symptoms, what can trigger them, medical diagnosis, and therapy. If you're ashamed about a bladder control problem, you may attempt to deal by yourself by using absorbing pads, bring added clothing or perhaps staying clear of going out. Infections of your urinary system tract or bladder may trigger temporary UI. When the infection is cleared, your UI will likely settle or improve.Urge Urinary Incontinence Pathophysiology
Exactly how to deal with hormonal agent imbalances?

Social Links